The New Frontiers in Veterinary Radiation Therapy
Advancements in veterinary radiation therapy are transforming cancer care for animals, bringing new hope and possibilities for their wellbeing. Offering increased precision with significantly reduced side effects, patients can maintain an excellent quality of life while achieving equivalent or better outcomes compared to older treatment protocols.
wellbeing. Offering increased precision with significantly reduced side effects, patients can maintain an excellent quality of life while achieving equivalent or better outcomes compared to older treatment protocols.
As technology continues to advance, veterinary professionals must stay updated about the latest state-of-the-art equipment and techniques—this is not the radiation therapy of generations past. By remaining at the forefront of oncologic treatments, veterinarians can provide enhanced cancer care options and significantly improve the lives of pet patients and their families.
“In the last decade, the field of veterinary radiation oncology has been reshaped by the introduction of two key technological advancements: beam-shaping technology and onboard imaging techniques. These innovations have overhauled the approach to treating cancer in animals with unprecedented precision and safety.”
The Evolution of Radiation Therapy
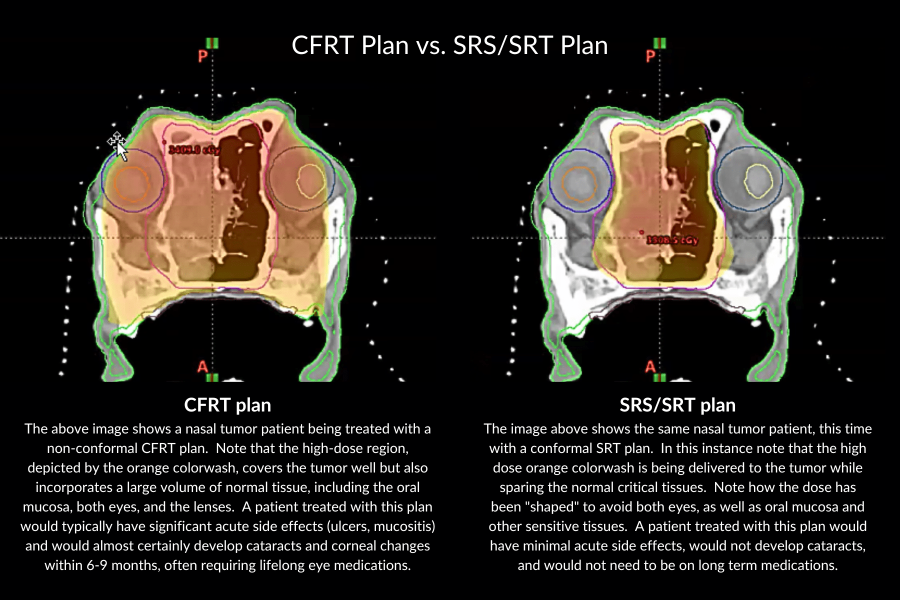
Historically, radiation therapy for animals suffered from significant drawbacks related to the inability to precisely target tumors. Lack of high-definition imaging options in early technology dictated that larger areas be treated in order to ensure the whole tumor was within the treatment field, causing damage to healthy tissues surrounding the tumor and leading to severe side effects. Because of this significant normal tissue damage, older treatment protocols necessitated dividing the radiation dose into 15-21 sessions, each one requiring general anesthesia to deliver—a major concern for both veterinarians and pet owners. Today, in the modern age of stereotactic radiation (SRS/SRT), advances in beam-shaping technology and onboard imaging capabilities have changed all of that significantly.
In the last decade, the field of veterinary radiation oncology has been reshaped by the introduction of two key technological advancements: beam-shaping technology and onboard imaging techniques. These innovations have overhauled the approach to treating cancer in animals with unprecedented precision and safety.
Beam-Shaping Technology
The advent of beam-shaping technology, and specifically the Dynamic Multi-Leaf Collimator (DMLC), has been pivotal to the transformation of radiation therapy. This technology offers the ability to adapt the shape of the radiation beam to conform exactly to the intricate contours of the tumor while safeguarding the surrounding healthy tissue. By programming the system to identify the treatment area as well as areas to avoid, the beam’s shape automatically adjusts the dose in real time as it makes its arc around the patient. This allows the delivery of a modulated radiation dose that can target the treatment directly to the tumor while minimizing exposure to nearby healthy sensitive tissues. The result is a significant reduction in side effects and the preservation of normal surrounding tissues.
Onboard Imaging (IGRT)
Image-Guided Radiation Therapy (IGRT) has brought about a leap in accuracy. This technology uses diagnostic CT scans to create highly detailed treatment plans and ensures that the tumor is precisely targeted. Custom immobilizers and indexing tables allow radiation therapists to place the patient in the exact same position each time treatment is delivered. This allows precise and reproducible positioning, greatly improving the delivery of the prescribed radiation dose to the tumor—especially in protocols requiring more than one fraction. Cone beam CT scans (CBCT) are taken immediately before treatment, which, when overlayed with the diagnostic CT images, allow for a pixel-perfect alignment. Thanks to IGRT, the number of anesthetic events required is significantly reduced, and complete treatments can be achieved in only one to three sessions.
Treating the Untreatable
These modern technologies have empowered veterinarians to recommend treatment for tumors that were once deemed untreatable. The exactness offered by these technological advancements has opened the opportunity to treat tumors located in sensitive areas of the body, including the adrenal glands, liver, lungs, heart base, spinal cord, and bladder. Today’s technology preserves sensitive tissues thereby drastically reducing risk of injury and side effects to the patient.
offered by these technological advancements has opened the opportunity to treat tumors located in sensitive areas of the body, including the adrenal glands, liver, lungs, heart base, spinal cord, and bladder. Today’s technology preserves sensitive tissues thereby drastically reducing risk of injury and side effects to the patient.
SRS/SRT vs. Conventional/CFRT
When compared to Conventional Fractionated Radiation Therapy (CFRT), Stereotactic Radiation, which can refer to either stereotactic radiosurgery (SRS) or stereotactic radiation therapy (SRT), offers a wide range of benefits all supporting the patient’s wellbeing. SRS/SRT’s advanced technology achieves superior targeting of the tumor and spares normal tissue. This precise delivery of the dose in SRS/SRT translates into a significant reduction in the number of anesthetic events and side effects. Whereas SRS/SRT requires one to three sessions, CFRT necessitates 16-20. Furthermore, an increasing number of studies and peer-reviewed articles note that outcomes from SRS/SRT are comparable to, or, in many cases, surpass those from CFRT.
The Critical Role of Experience in SRS/SRT
Experience is crucial when it comes to effectively administering SRS/SRT, and utilizing this advanced technology involves a steep learning curve even for a highly trained radiation therapist. They must determine the appropriate dosage for each individual patient and understand its limits.
Despite the precision of this new technology, mistakes are still possible, and they can lead to serious injury or even death. For example, exceeding the correct dose in the treatment of a thoracic spinal lesion could result in paralysis. Therefore, experience of the radiation therapist who operates this advanced equipment is of paramount importance.
What to Look for in an Advanced Cancer Treatment Facility
Before referring patients for advanced cancer treatment, veterinarians should familiarize themselves with the cancer treatment facility’s staff, capabilities, and history. Consider researching the following:
- What are the qualifications and certifications of the oncology staff, and does the team include board-certified veterinary radiation oncologists, radiation therapists, and medical oncologists for comprehensive care?
- How long has the facility been performing SRS/SRT, and what volume of patients do they treat annually?
Does the facility use beam-shaping technology and onboard imaging systems, and can they provide evidence of their expertise in these technologies? - What protocols are in place for quality assurance and patient safety during radiation therapy, especially for adjusting treatments in response to unexpected changes? (Consider the changing nature of a pet’s bladder.)
- How does the facility manage communication with referring veterinarians?
Asking these questions can assist in understanding a facility’s capacity to deliver safe, precise, and successful SRS/SRT treatments, ensuring the best possible care for referred patients. Veterinary radiation therapy has come a very long way in the last decade and, at times, feels like a science fiction movie come to life. The tools we have today bear little resemblance to the tools of the past and have the potential to treat what was once considered beyond the reach of veterinary medicine. Today, the field of veterinary oncology offers real hope and healing with minimal side effects and stress to the patient.
For veterinary professionals, understanding these technologies, their application and potential, and recognizing the importance of expertise in their usage is central to the quality of care we provide in this advanced and rapidly evolving time of veterinary oncology.
Dr. Neal Mauldin, Chief Veterinary Medical Officer at PetCure Oncology and the National Director of Radiation Oncology for Thrive Pet Healthcare, is a pioneer in the field of veterinary oncology, having supervised the treatment of over 8,000 pets with stereotactic radiation (SRS/SRT) since 2010. With triple-board certification in internal medicine, medical oncology, and radiation oncology, his over 37 years of experience include roles at VCA Canada Western, the Animal Medical Center in New York, and Louisiana State University. A former president of the Veterinary Cancer Society, his training spans Texas A&M University, the Animal Medical Center, and a fellowship at Memorial Sloan Kettering.
